Medical billing is one of the most critical functions of any medical practice. As a result, many practice managers and leaders place a high value on the effective administration of their medical billing, account receivables and overall revenue cycle management (RCM). Either you can pay full-time employees to handle your medical billing. Or, you can outsource it to a third-party medical billing service, such as CPa Medical Billing (CPaMB), that possesses the expertise and manpower to maximize the practice’s financial health.
Medical billing is one of the most critical functions of any medical practice. As a result, many practice managers and leaders place a high value on the effective administration of their medical billing, account receivables and overall revenue cycle management (RCM). Either you can pay full-time employees to handle your medical billing. Or, you can outsource it to a third-party medical billing service, such as CPa Medical Billing (CPaMB), that possesses the expertise and manpower to maximize the practice’s financial health.
So, which option is right for you? While your costs will largely depend on practice volume, software systems, specialty etc., we’re happy to give you some ballpark figures to mitigate any surprises throughout the decision-making process.
In-house medical billing service costs
Typically, in-house medical billing costs range from 7% to 10% of total net collections. This percentage includes salaries, benefits, operational costs and overhead (office space, computers, phones, internet, software, desks, office supplies, etc.).
Beyond the obvious costs, there are a few other factors to consider which significantly increase your time and cost to manage in-house staff. Operational costs such as recruiting, training, effective management, reporting, reviews, paid time off and more need to be included in the calculation to determine costs.
In summary, in-house medical billing services can be an expensive option when you tally up every line item.
Outsourced medical billing service costs
Medical billing companies typically charge a percentage of net collections ranging from 4% to 10%, with 5% to 8% being the most common range. The percentage variance is rather large because there are so many factors that affect your final pricing.
Here are a few areas that a professional medical billing companies will consider when developing a pricing quote to handle medical billing services for your practice:
Where will the billing work be performed?
Many medical billing companies outsource aspects of their own operations to offshore companies, commonly in India or the Philippines, as a way to cut overhead costs. When work is performed offshore, the fee for services is much less because full-time employees in those countries range from $800 and $1600 per month. In the U.S., a full-time medical biller may cost between $3500 – $5000 per month.Outsourcing overseas is not uncommon, however it’s important to understand how it can impact your costs – and your patient experience.
(Pro Tip: If you’re concerned about having offshore medical billers, don’t hesitate to ask for IRS form 941, which illustrates exactly how many US-based employees a company has on their payroll. Many billing companies will have a US office and tell you their company is US based, but when you look into the 941, it may only show a handful of employees are located in the US.)
How do billing systems help determine price?
The billing systems play a role in determining price. While newer, sophisticated systems are highly efficient and run almost everything electronically, others lag behind when it comes to electronic processing and the plug-in enhancements compatible to the system. The more the system can process electronically, the lower the fees.
(Pro Tip: Ideally, your billing partner is an expert with your practice management software. A top-tier medical billing company like CPaMB works within most major practice management systems including EPIC, Centricity, NextGen, eClinicalWorks, Intergy, Allscripts, Modernizing Medicine, Dentrix, etc.)
What is your monthly medical billing volume?
The number of patients seen increases claims generated which will drive your volume. The higher your volume, the lower your outsourced billing rate will be.
What is your specialty & average reimbursement per claim?
Essentially, the lower your practice’s average reimbursements are, the higher the billing fees will be. For example, physical therapy (PT) claims have low reimbursement rates while orthopedic claims deliver high reimbursement rates. A PT practice can expect a higher billing fee than an orthopedic practice.
Which type of medical biller is being used? A specialist or generalist?
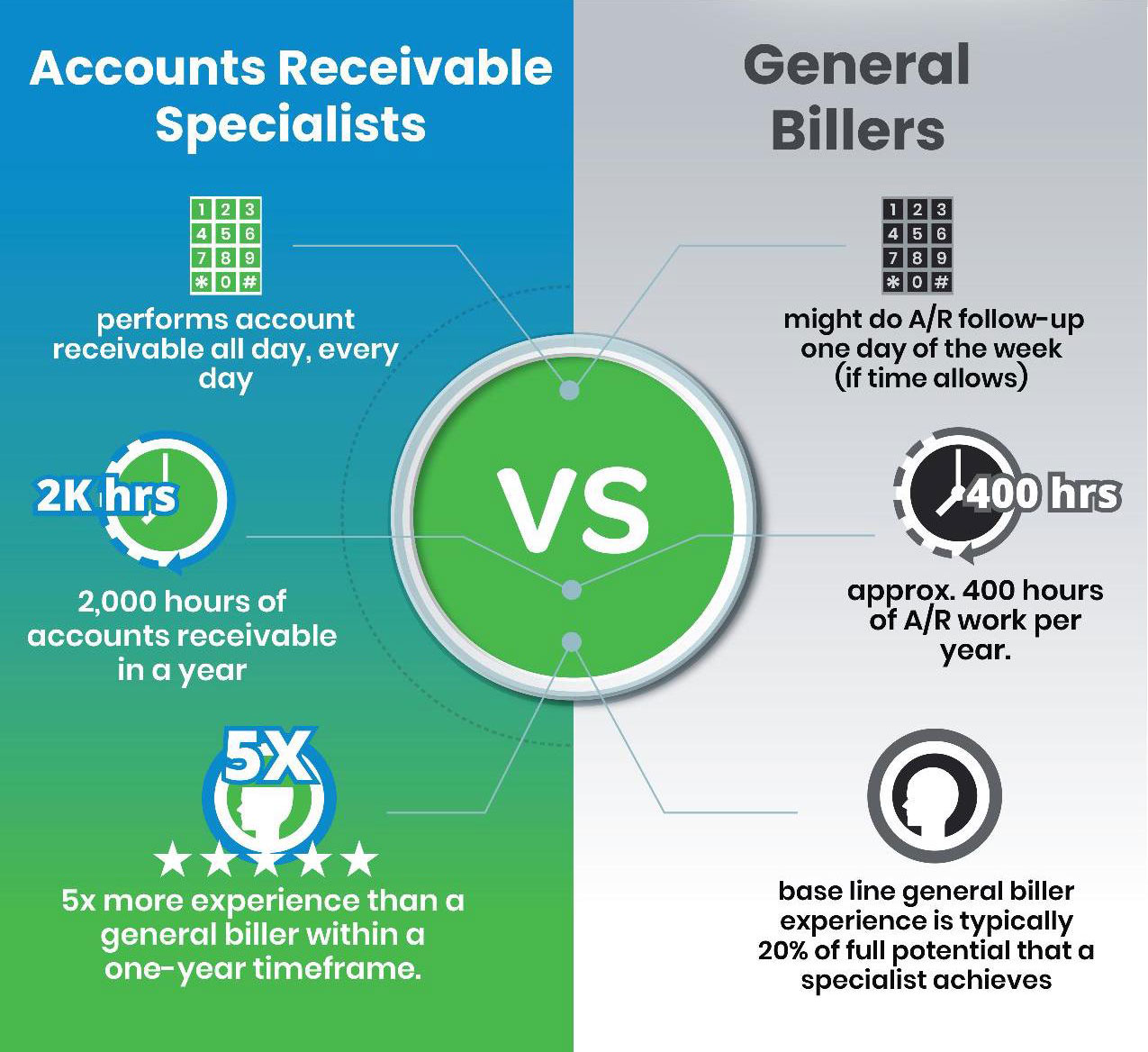
A generalist is a person who can perform multiple components of RCM whereas a medical billing specialist is someone who can perform only specific components of RCM.
Many medical practices are quick to hire the generalists, but this can lead to costly mistakes. More often than not, generalists lack the experience and expertise needed to boost your bottom line. A medical billing specialist can log more A/R hours, moving quickly and efficiently.
Will you receive verified or unverified results?
Ensure that your medical billing company shares measured performance statistics, case studies and client testimonials to ensure you’re getting the best return for dollars spent. You can even ask for past client references and contact information. Performing a significant amount of due diligence (and not just take the company’s word that they’ll do a great job) is a critical part of identifying the best company to provide medical billing services.
Other questions related to the cost of medical billing services
- Is in-house medical billing better than outsourced medical billing?
It all depends on the people and processes. From our experience in evaluating the medical billing structure for hundreds of private practices and health centers (FQHCs and CHCs), outsourced medical billing delivers better results roughly 90% of the time. An outsourced medical billing company should provide a positive ROI, meaning that the results they produce for your practice are going to pay for themselves. It should also provide your practice with additional income (by having a team of medical billing experts) that is rarely obtained with an in-house medical billing team. Moreover, outsourced medical billing always increases your cash flow as you pay the medical billing service fees AFTER you collect your reimbursement. An inhouse staff requires prepaying for almost all of the expenses. - How long does it take to get a quote for outsourced medical billing?
Obtaining a quote for medical billing services should take no longer than 1-2 business days. The medical billing company will most likely ask you to share a few details such as what software is being used, how many offices, how many providers, your medical specialty/specialties, payor mix, aging A/R, annual visit count and annual net receipts.
Did you enjoy this article? Check out additional articles here:
9 Reasons Medical Practices Should Outsource Medical Billing
The Ultimate Guide to Outsourced Medical Billing Services
Contact CPaMB for a Free Quote
As with any major consideration, it’s important to take your time investigating the right solutions and vetting potential partners. Finding a highly specialized and experienced partner can make a world of difference for you, your practice, your patients– and your overall revenues.
Since 2003, CPa Medical Billing (CPaMB) has elevated the financial health of private practices, health centers, and medical groups across the U.S. Our highly trained, highly experienced medical billing specialists are all US based and operate together from in one office. Our engagements are flexible and tailored to your specific needs.
If you have questions or would like to get a free quote, please call 203-678-9616 or visit https://cpamedicalbilling.com/contact-us/